So here we go…
Soon after my last post, in March of 2020, COVID came to Australia and we began a strict, 3 month lockdown. I was required to work from home on my PhD and my husband was stood down from his position (meaning put on leave without pay). My dream of living abroad quickly turned into a scary limbo of financial insecurity and the realization that I likely wouldn’t be able to just jump on a plane to go see my family for the foreseeable future. While those three months provided me a lot of wonderful time with my husband, it also brought back so many memories that I was not prepared for. The idea of working from home and having to remain socially isolated scared me because of how much those same things had negatively impacted me during my treatment. Part of my brain wanted to just shut down at the thought of having to stay in my apartment for three months, with no social contact, yet still having to be productive. My anxiety led me to prepare for the worst – impending depression, loss of friendships and more - and yet I quickly realised that this time would be very different. The fact that everyone had to isolate along with me made such a difference. And it made me wonder what the social futures of cancer patients could look like, and how much better they could be now that everyone is so comfortable with Zoom and online games.
Fortunately, Australia’s lockdown got things under control and they were able to begin lifting restrictions in June of 2020. Just as things were looking up, I was confronted with the unfortunate reality of having to pursue fertility preservation because my fertility specialist indicated I likely would not be able to naturally conceive for much longer (I was given about a 2 year window). I was likely headed for menopause before the age of 30. I had been able to put it off during the lockdown, when elective procedures were put on hold. But, with the lockdown lifted, I had no choice but to delve into what I soon realised was an extremely scary and overwhelming world of helplessness. For me, fertility preservation felt important because I was only 25 and even though I was married, I wanted so much to finish my PhD first. I also didn’t feel like I had finished being young yet. I had spent so many years of my life wanting to be a young adult, where how mature I felt and my interests would finally match up with my age and the interests of my peers. The last 2 years had been so joyful, making new friends and doing fun things in this beautiful new country I was in, I didn’t feel ready to be a parent and be responsible for a tiny human yet. While my husband and both knew we would eventually want kids, we didn’t quite feel ready. So, we decided to give IVF a try, and freeze embryos we could use in the future. I mentally prepared myself to confront injections and invasive procedures. I tried to maintain the positive and remain optimistic. My specialist also assured me that I was young and this would likely be a successful procedure, although there were no guarantees. But, one of the things I forgot about was how inclined I was to latch on the positive, assuring words of a healthcare provider and tune out the risks and complications. In latching on to her words of assurance, I went into my first IVF cycle feeling so sure everything would work out. I talked about it with my family and friends, and I felt so confident about the outcome. I was young and healthy after all, and so was my partner. There were no clear reasons this shouldn’t work for us as far as we understood.
But, 5 days into my first cycle, after getting over the fears of once again doing home injections, and the memories that resurfaced along with the smell of alcohol swabs and the stings of sharp needles, I thought I’d be ok. That I’d get through it. But then, I got a phone call. My hormone levels had risen properly, but the ultrasound only showed one mature egg in one ovary, when we needed at least 5-10 in each ovary. It wasn’t clear why this happened when everything else had looked right. I was advised to stop that cycle and restart the following month with a different combination of drugs. Not only did the financial pressure of already spending $4000 on medications make this a big blow, but it brought out emotions I didn’t expect. Feelings of anger that somehow I, as a woman, was unable to do the one thing I’m supposed be born able to do. Feelings of guilt that this may mean I may not be able to give my husband children (even though he constantly reassured me that has never been a concern for him, and my wellbeing is a priority - he’s happy to take other routes to parenthood if we needed). And feelings of helplessness because something that should have worked didn’t, and no one really had an answer for why. So we continued on, and I spent 3 weeks recovering before beginning a new cycle. I tried to return to optimism and hope that it would work out. Then, five days into the second cycle, I got another phone call. Again, the same problem, although slightly better results. Only 2 mature eggs appearing in one ovary, and one in the other. I was given the choice to cancel again, but it was likely that if I hadn’t responded twice, a third time would not be any different. So, I was advised to proceed to the egg retrieval stage to at least try to get a few eggs. So, we forged ahead and I went in for the egg retrieval. I woke up from the anaesthesia to be greeted by the concerned face of my specialist. They had only retrieved one egg. I was so delirious I couldn’t feel crushed, but I knew I was. I just went home and cried, waiting for the call from the laboratory in two days’ time, to find out whether our one chance fertilised.
Then the call came: it fertilised but was abnormal so would not result in a viable pregnancy. I then got a call from my specialist. She was very kind and supportive and apologised that this didn’t work out even though she had hoped it would. But, then she began sharing some interesting information she had left out before. Turns out she had had 3 other young female patients who had been diagnosed around the same age as me and had experienced similar complications during the IVF process for reasons no one could explain. My specialist clarified, there is just a lot they still do not know about the impact of adolescent (teenage) cancer on fertility and fertility preservation processes. Surprisingly, she said all three of those girls were able to naturally get pregnant in the year following their failed IVF cycles. I was shocked. I know healthcare providers weigh up what information is best to share with patients and have to make a decision about what to share, but so much of me had wished she had told me those stories before I began all of that so that I could have been more prepared. I felt I would have rather been worried about facing those similar outcomes, than to experience the helplessness and guilt I did. But, at least now I had some kind of reason. Something happened during treatment that made me not respond to this process, although no one knows exactly what.
So, my husband and I were advised to start trying to get pregnant within the following 6 months, and to check in with the specialist again if we couldn’t after 6 months of trying (because my window of opportunity was getting smaller). Even though we weren’t 100% ready, we knew this could be our only chance, so we decided to go ahead. By some miracle (and a LOT of calculation and structured timing of things), after only 3 months, I found out I was pregnant in November of 2020. I was shocked and rather scared because, even though I knew we were trying, a huge part of me just expected it not to work. Fast forward to now, April 2021, and I’ve made it more than halfway, expecting a healthy baby boy in July. While we don’t know what the future looks like in terms of my ability to get pregnant again, and I didn’t feel entirely ready to be a parent, I feel so lucky that this little miracle happened.
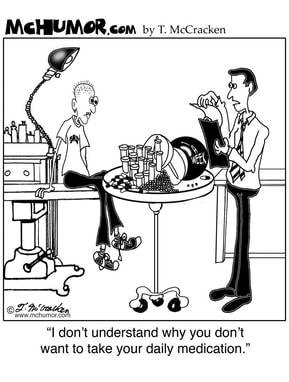
And I’ve learned about the disadvantages of focusing too much on the positive and not preparing enough for the challenges. I’ve learned that sometimes you need to vent and be angry, that while emotions can be painful, they have to be felt to move forward. I’ve learned to ask more questions from healthcare providers too, like what’s your experience been with outcomes for other young women like me?
I’ve also been reminded how important it is to channel emotions raised from cancer and survivorship experiences into something you love doing, to take your mind off your own struggles and to find joy in doing something. Through my PhD work, I’ve gotten to speak with and survey young people currently going through treatment or recently finished treatment. I’ve spoken with people about their toughest moments and laughed with them about their funny stories. I spend my days reading and writing papers with the goal of calling attention to what future research and improvements in care need should focus on. I’ve immersed myself into this community that I love so much, and it’s brought me so much joy to feel so connected and to have such a sense of purpose. More importantly, thanks to the young people I meet, I can continually be reminded that I’m not alone in all of this 😊 Even 12 years after finishing treatment, the twists and turns of the survivorship roller coaster make me especially grateful for reminders that I’m not alone and there’s still so much important work to be done for this amazing community of young people.
I'd love to hear from you about your challenges, triumphs and lessons learned over the past year - share your thoughts in the comments below!



 RSS Feed
RSS Feed

