As I am relatively new to Twitter, I had never heard of a Twitter chat before and I certainly had no idea how it would work. But, when I logged into my Twitter account at 1pm for the beginning of the chat, I was blown away.
What a way to bring people together to talk about important issues! While Twitter does pose a bit of a challenge due to its character limit, I was amazed at how many people and organizations responded in useful ways to the questions posed by the NCI and NIMH. I was also pleasantly surprised by the amount of focus given to adolescent and young adult cancer coping issues.
If you are a teen or young adult going through cancer treatment or just starting life as a survivor, you should get on Twitter. I highly recommend following the NCI @theNCI, the AYA cancer organization Critical Mass @heycriticalmass, and the American Psychosocial Oncology Society @APOSHQ. They often post useful cancer care and coping information/resources.
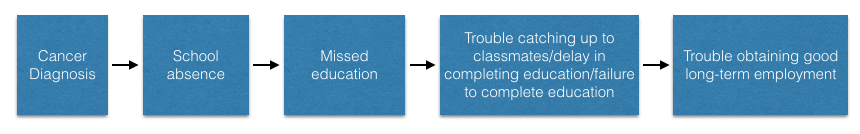
That being said, there was also one MAJOR issue I noticed through participating in the #CancerCoping Twitter chat. All the experts and hospitals participating seemed to recognize that the psychosocial challenges cancer patients (of any age) face during treatment warrant quality care. This was especially the case when the psychosocial needs of adolescents and young adults were brought up. However, when the final question of the chat asked what patients can do to get help or find resources, I did not see many responses relevant to AYA psychosocial health. While many organizations offer support resources - booklets, videos, information, etc. - I did not see any hospitals mention care programs designed to serve the psychosocial needs of AYA patients going through cancer treatment.
For example, here is one comment by the NIMH that I responded to:
So, where is the disconnect? If the NIMH makes such a comment, why have major hospitals still not instituted clear psychosocial care programs for AYA patients?
In my own case, I wonder if the hospital "thought" they were providing me such care by providing a social worker to help my family and I. The problem with that, however, was that the social worker was rarely around on the days I came to clinic/the hospital and I was never sat down for a one-on-one psychosocial interview. Fortunately I did not have any serious mental health issues to contend with during my treatment. But, what if I had become depressed because I did not know how to cope with my relapse diagnosis? As it was I had trouble figuring out (on my own) what coping even involved and how I could do it through the various stages and challenges of cancer treatment and survivorship. It definitely would have been nice to have a professional there to guide me through that.
That being said, my lesson learned from today's Twitter chat is:
The #CopingCancer world is definitely making important steps towards recognizing and supporting the psychosocial needs of cancer patients. However, there are still steps to be taken to ensure that all patients, and AYA patients in particular, are provided proper psychosocial care from beginning of treatment through survivorship.
While I have found it incredibly wonderful to write this blog and share my favorite resources through Twitter, patients and survivors should not have to go fishing through Twitter feeds or scrolling through blogs like this one, to find answers or support.
One day I hope to be a clinical psychologist and work to develop or enhance psychosocial care for AYA cancer patients and survivors. I will cross my fingers that such programs will be much more common by that time :)
 RSS Feed
RSS Feed

